An amended version of the 1915(b)/(c) Innovations Waiver (Waiver) for individuals with intellectual and developmental disabilities took effect on November 1, 2016. The Waiver amendment included new assessment tools and terminology.
This guide will explain some of the changes to the Waiver rules, including how your Individual Budget is developed, your right to request services in excess of your Base Budget, and tips on completing your Individual Support Plan (ISP).
Your Individual Budget
The Individual Budget consists of two types of services—Base Budget services and Non- Base Budget services. The letter you receive from your LME/MCO about your budget only refers to the costs of Base Budget Services, and the amount is not supposed to limit what services you can request or receive.
Base Budget Services are core habilitation and support services:
- Community Networking Services
- Day Supports
- Community Living and Support (includes services previously called In-Home Skill Building, In-Home Intensive, and Personal Care)
- Respite
- Supported Employment
Non-Base Budget Services are preventative services and equipment:
- Residential Supports (services that enable someone to live in a group home or Alternative Family Living setting)
- Supported Living (a new service that allows someone to remain in their home with daily service or the help of a live-in caregiver)
- Assistive Technology Equipment and Supplies
- Home Modifications
- Vehicle Modifications
- Community Navigator (previously named Community Guide)
- Community Transition Services
- Crisis Services
- Financial Support Services
- Individual Goods and Services
- Natural Supports Education
- Specialized Consultation Services
Your Individual Budget is based on:
- Your age – are you a child or an adult?
- Your place of residence – do you live in a group home, other Medicaid-funded home, or a private home?
- The kinds of supports you need as measured by the Supports Intensity Scale (SIS)
What Can I Do If My Budget Has Been Reduced?
Many individuals on the Innovations Waiver have received letters from their Local Management Entity/Managed Care Organization (LME/MCO) suggesting that their Base Budgets will be reduced over the next one to three years.
The Base Budget you have been assigned is NOT supposed to be a limit on the amount of services you can request or receive. It is supposed to be a guideline only. You should request services in any amount and duration that you believe meets your needs, even if the requested services will cause you to exceed your assigned Base Budget. You always have the right to ask for all of the services and supports that you believe are medically necessary.
Supports Intensity Scale (SIS)
The SIS is designed to evaluate general, medical, and behavioral needs, and is administered when an individual enters the Waiver program. SIS re-assessments occur every two years for participants between the ages of 5 and 15 and at least every three years for participants 16 years of age and older. All Waiver participants must have their support needs evaluated through the SIS.
A SIS interviewer will come to your home to administer the SIS. He or she will go over questions about your mental, emotional, and behavioral needs. While the SIS was not designed to be used for setting budgets, the information gathered by the interviewer will be used to establish a score that will have a significant effect on your Base Budget. To be sure all helpful information is included, you should have family members and/or care staff present to help answer the interviewer’s questions.
An example section of the Supports Intensity Scale
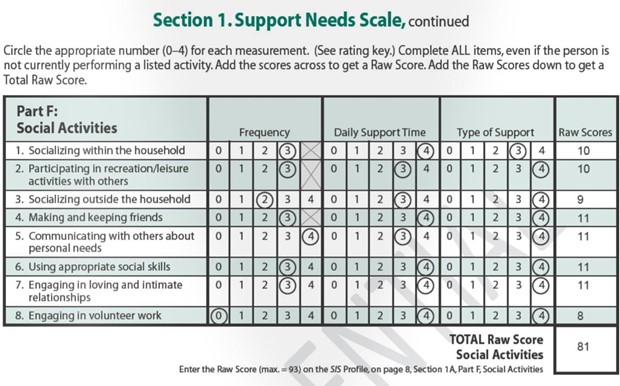
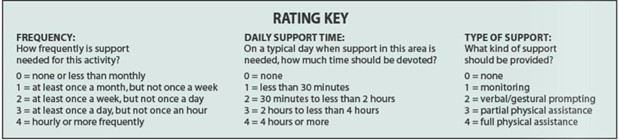
Once you get your SIS score, the SIS interviewer or your Care Coordinator will schedule a time to go over the results with you, your family, and, if necessary, your service providers. If you have questions or concerns about your SIS, notify the SIS interviewer or Care Coordinator immediately. The SIS interviewer or Care Coordinator should inform you of how to proceed to get your questions or concerns resolved.
Individual Budgeting Tool
The Individual Budgeting Tool (formerly called the Support Needs Matrix) takes into account:
- Your living arrangement (do you live with family or in a community residential setting) and age, which correspond to a Budgeting Category, plus
- Your SIS score, which is used with an algorithm determine your Level (A to G) within the category.
Budgeting categories and levels
All Waiver participants are assigned to one of four Budgeting Categories, based on age and living arrangement. The four categories are:
- Non-Residential Child (under 22 and living in a private home);
- Residential/Supported Living Child (under 22 and living in a group home, an Alternative Family Living setting or a Supported Living setting);
- Non-residential Adult (age 22 and over and living in a private home); and
- Residential/Supported Living Adult (age 22 and over and living in a group home, Alternative Family Living setting, or Supported Living setting).
Each category has seven Levels. The Levels are on a scale from A to G, with A representing the lowest need for services and G representing the highest need for services. Your Level is based on your SIS results.
Each Budget Category and Level (A to G) is associated with a preset dollar amount. It is not an individualized determination of your particular needs, which will be different for everyone based on what is medically necessary for you. It is important to include all relevant information and supporting documentation when preparing your ISP request so that an accurate amount of services can be approved for you.
Your Budgeting Category and Level are used to determine your Base Budget. Remember, however, that the Base Budget is not supposed to be a limit on the total costs of services that can be authorized in your ISP. Although Disability Rights NC has seen indications that Base Budgets are being used as a basis for denials, your Base Budget should not be a hard limit or cap on the amount of services you can request or be authorized to receive. If your Base Budget is used to deny you services, please contact Disability Rights NC.
Also, your Base Budget does not include the costs of Non-Base Budget services, such as Residential Supports, Supported Living, Home Modifications, and other services.
Requesting a Change to Your SIS Results
If you have questions or concerns about your SIS results, you should contact the LME/MCO within 30 days of receiving the SIS score. However, even if you fail to object to the SIS within 30 days does, you can still contest the results when requesting services or in an appeal.[1] A SIS interviewer should call you to review the SIS summary and answer your questions. If your concerns are not answered during your telephone call, you may request a meeting with the SIS interviewer to discuss the results and possibly request a new SIS.
Three ways you can request a change to your SIS results
Request a new SIS
After the face-to-face meeting with SIS interviewer, you may request a new SIS if you feel that the SIS does not accurately reflect your support needs. The MCO has 90 days from the date of the request to schedule and perform a new SIS. The MCO must also inform you of your right to file a grievance. You also can challenge the correctness of the SIS evaluation when requesting services or during a service appeal.
Request an addendum:
An addendum may be added to the SIS if one or more of the ratings on the SIS do not accurately reflect your support needs. The SIS interviewer or Care Coordinator can provide you with assistance in documenting your concerns. If it is determined through review of the results and any additional information provided that the SIS results do not adequately capture your support needs, the SIS interviewer or Care Coordinator will meet with all concerned and prepare an addendum to the SIS (the original SIS is not altered). You will receive written notification (including a copy of the SIS and addendum) by mail letting you know if the addendum has been approved.[2]
Request a re-assessment
You may request a re-assessment at any time when a major life change occurs. Major life changes include, but are not limited to the following:
- An emergency or crisis in your living situation, such as the loss of housing or the loss of a primary caregiver;
- Repeated incidents in which your health and safety or someone else’s health and safety were in jeopardy;
- A new diagnosis of a serious mental health condition; and
- Transitional changes, such as moving to a more independent living. [3]
[1] Clinical Coverage Policy 8 P, p. 117-118, Amended 11/1/2016
[2] Clinical Coverage Policy 8 P, p.118-119, Amended 11/1/2016
[3] Clinical Coverage Policy 8 P, p.118-119, Amended 11/1/2016
NC Division of Medical Assistance Clinical Coverage Policy 8-P
Your individual support plan (ISP)
Your assigned Individual Budget is not a cap on the costs of services and supports you can receive through your Individual Support Plan (ISP). You should request all services covered under the Innovations Waiver, including Residential Supports and Supported Living, that are medically necessary, regardless of your Budgeting Category.
You may request services that cost more than your Individual Budget if your needs cannot be met within that budget. A Care Coordinator must assist you in requesting all of the services you want in the ISP, regardless of any limits on sets of services or the Individual Budget. In other words, LME/MCO staff are required to draft an ISP that includes everything you want to request. A Care Coordinator may explain alternative service options that may be appropriate, but you get to decide what services are requested in your ISP.
If the LME/MCO determines that it is medically necessary for you to have services that cost more than your Individual Budget, the LME/MCO is required to authorize those services. If a request for services is ever denied partially or fully, then the LME/MCO must notify you of the reason for the denial and how to appeal the decision.
What is Medically Necessary?
Medicaid only provides services that are considered “medically necessary”. The federal government defines medically necessary as “health care services or supplies needed to prevent, diagnose or treat an illness, injury, condition, disease or its symptoms and that meet accepted standards of medicine.”[4]
[4] Centers for Medicaid & Medicare Services, Uniform Glossary of Health Coverage and Medical Terms
It’s the Law – You Cannot Be Discouraged from Requesting Services
In order to protect participants from intimidation and discouragement, Care Coordinators or other staff members may not:
- Tell you that you cannot request a particular service or suggest that the amount, frequency or duration (within a Plan Year) of a particular service must be less than 12 months;
- Threaten to retaliate against you if you choose to appeal a denial of services;
- Threaten to force you to pay the cost of continuation of benefits;
- Tell you that you must sign an ISP with which you do not agree; or
- Ask you to sign a blank or incomplete
You should insist on your right to submit a plan containing all services you want to request, regardless of your SIS score, budget limits, or limits on sets of services. LME/MCO staff should assist you in requesting the services you need. If they do not, they may be violating the law.
To Sign or Not to Sign the ISP
You WILL need to sign the ISP in order to continue receiving services. However, you should NEVER sign a plan that does not include all of the services you need. Insist that the Care Coordinator include all of the services you need in the ISP, regardless of whether the Care Coordinator believes the services will be approved. It is a violation of the law for a participant to be told that he or she must sign an ISP that does not contain all of the services the participant wishes to request.
You must be allowed to request that services be authorized for the entire plan year. Additionally, you have the right to make a new request for services at any time during the plan year by requesting an update to the Plan of Care, sometimes called a Continuing Need Review (CNR).
Objecting to Your ISP
You will have two opportunities to object or indicate disagreement with the services requested when you sign the ISP. You should document any issues or disagreements that you have with the way the ISP is written in one or both places on the signature page.
You can document your objections in the Statement of Concern or Disagreement box, which states:
“I, the individual/legally responsible person signing this plan, have concerns or disagree with the following issues related to my Individual Support Plan.”
Beneath this statement, there is space for you to list or explain the problems.
Additionally, when you sign in the box that says Update to ISP Signatures, you can cross through statements with which you disagree. That box reads as follows:
“By signing this plan, I am indicating agreement with the bulleted statements listed here unless crossed through. I understand that I can cross through any statement with which I disagree:
- My care coordinator helped me know what services are
- I was informed of the range of providers in my community qualified to provide the service(s) included in my plan and freely chose the providers who will be providing services/supports.
- This plan includes the services/supports I need.
- I participated in the development of this plan
- I understand the PIHP (prepaid inpatient health plan) will be coordinating my care with the PIHP network providers listed in this plan.”
Be sure to cross out any of the above statement(s) with which you disagree and note any issues with the ISP before signing the form. You will not lose appeal rights by signing the form—as long as you document your objections.
We hope this information is helpful to you. If you believe that the LME/MCO violated your rights related to the SIS or ISP, please contact Disability Rights North Carolina.
