Executive Summary
The State of North Carolina lacks adequate services and systems to support people with Traumatic Brain Injury (TBI). It lacks even basic data about the location and needs of TBI survivors. The state’s own publications support these conclusions.
People with TBI can benefit from a wide range of therapies and supportive services. While these needs are most acute in the months immediately following a TBI, needs can persist for years, even for life. Recent efforts to increase access to services in North Carolina have not been successful. To correct course and move the state toward meeting the needs of North Carolinians with TBI, Disability Rights North Carolina (DRNC) recommends that the state:
- Invest in Identifying People with TBI and Their Needs
- Invest in the Creation of a High-Quality Network of Providers
- Implement Long-term Case Management for People with TBI
North Carolina’s InAction Plan
The North Carolina State Action Plan for People with Traumatic Brain Injury for 2021 [1] was written and released by the North Carolina Department of Health and Human Services’ Division of Mental Health, Developmental Disabilities and Substance Abuse Services (NC MH/DD/SAS). It notes that Traumatic Brain Injury (TBI) is an issue for a large number of individuals in North Carolina and that TBIs are a common cause of emergency department visits in our state.
[1] North Carolina State Action Plan for People with Traumatic Brain Injury, https://files.nc.gov/ncdhhs/TBIStateActionPlan_FINAL.doc
The state plan includes this sobering paragraph:
This paragraph is an urgent call for action to address many serious concerns regarding the wellbeing and rights of people with TBI in North Carolina. However, a similar paragraph was in the state’s 2017 action plan for people with TBI. This sad and frustrating fact is clear evidence of the lack of progress North Carolina has made in creating a system of care and supports for people with TBI.
North Carolina has taken one important step forward—the creation of a TBI Medicaid waiver initiative program. But the initiative serves only 4 of the state’s 100 counties, and North Carolina’s historical failure to track people with TBI and its continued lack of investment in the development of an adequate provider network have significantly hampered the effectiveness of the waiver program. As a result, only a handful of the thousands of people with TBI in North Carolina receive services specific to their needs.
What is Traumatic Brain Injury?
“A traumatic brain injury (TBI) is an injury that disrupts the normal function of the brain. It can be caused by a bump, blow or jolt to the head or a penetrating head injury. Explosive blasts can also cause TBI, particularly among those who serve in the U.S. military. The number of individuals surviving traumatic brain injury has been rising with the advances in trauma care…
“TBI can be categorized as mild, moderate or severe based on the extent and nature of the injury, duration of loss of consciousness, post-traumatic amnesia, and the severity of confusion at the initial assessment during the acute phase of the injury. These labels describe the extent of neurological injury to the brain and are not necessarily reflective of the extent and functional deficits or predictive of the recovery from the injury. Service needs for these individuals may span the spectrum of medical, behavioral, cognitive, educational and vocational services.”
North Carolina State Action Plan for People with Traumatic Brain Injury
Disability Rights NC’s Survey of People with TBI
As NC’s federally mandated Protection and Advocacy agency (“the P&A”), Disability Rights NC provides legally based advocacy services to people with disabilities, including those with TBI. In this role, people with TBI and their families reach out to DRNC with heart-breaking, frustrating experiences of a system that fails the needs and rights of this unique population.
Disability Rights NC wanted to better understand the perspectives of people with TBI and their experiences with North Carolina’s system of care, including the prevalence and consequences of failing to provide necessary TBI services and supports. This examination revealed long-standing systemic neglect that unnecessarily, and in some cases illegally, forces many people with TBI to rely on families, loved ones or institutions for their care and support.
This conclusion and report is largely based upon the work of Travis Glass, MS, LCMHC, CBIS, a clinician in North Carolina who specializes in TBI, with whom DRNC contracted to interview people with TBI and professionals who work with people with TBI from around the state. These individuals brought up the same issues highlighted in the paragraph from the state plan cited above, confirming:
- Inadequate provider networks
- Lack of knowledge in the provider community about TBI and its long-term effects
- Shortage of appropriate community-based services and support
We also conducted an online survey of people with TBI and caregivers. In analyzing the 134 responses we received, we saw similar patterns regarding the need for more providers and services.
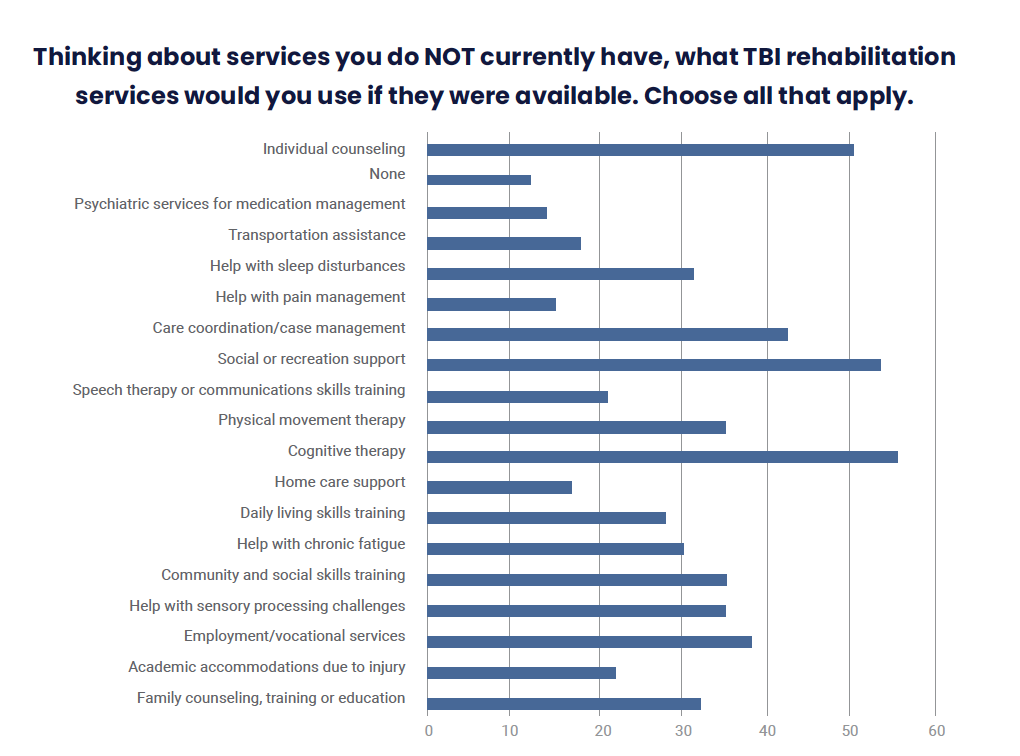
For example, 77% of respondents identified at least one rehabilitation service that they need but do not have access to. The services most commonly identified as being needed but not available relate to gaining the skills required for a good quality of life, such as:
- Cognitive therapy for attention, memory, initiation, problem solving, planning, and other issues
- Social or recreation support to help with interactions with others and to address loneliness
- Individual counseling for treatment of depression, anxiety, anger, or substance abuse
- Employment and vocational services for help getting and/or keeping a job
Survey Results: Services and Supports
Answers from people living with TBI in North Carolina in response to the question: “What supports or services not covered in this survey would be useful to you?”
- How to keep families together and work through marriage with loved 1 with TBI.
- I need someone to help me find resources to help with daily living.
- I need vocational assistance and it is unavailable.
- I would like to live on my own but need some help with chores (learning to do things in my new home, some social skills, better job, transportation help especially to college).
- Independent living with adequate support. Permanent employment with companies that understand and work well with TBI sufferers.
- Teaching organization and computer even cell phone or things that would help make life much easier. Great to have someone to help come in home and help organize with me.
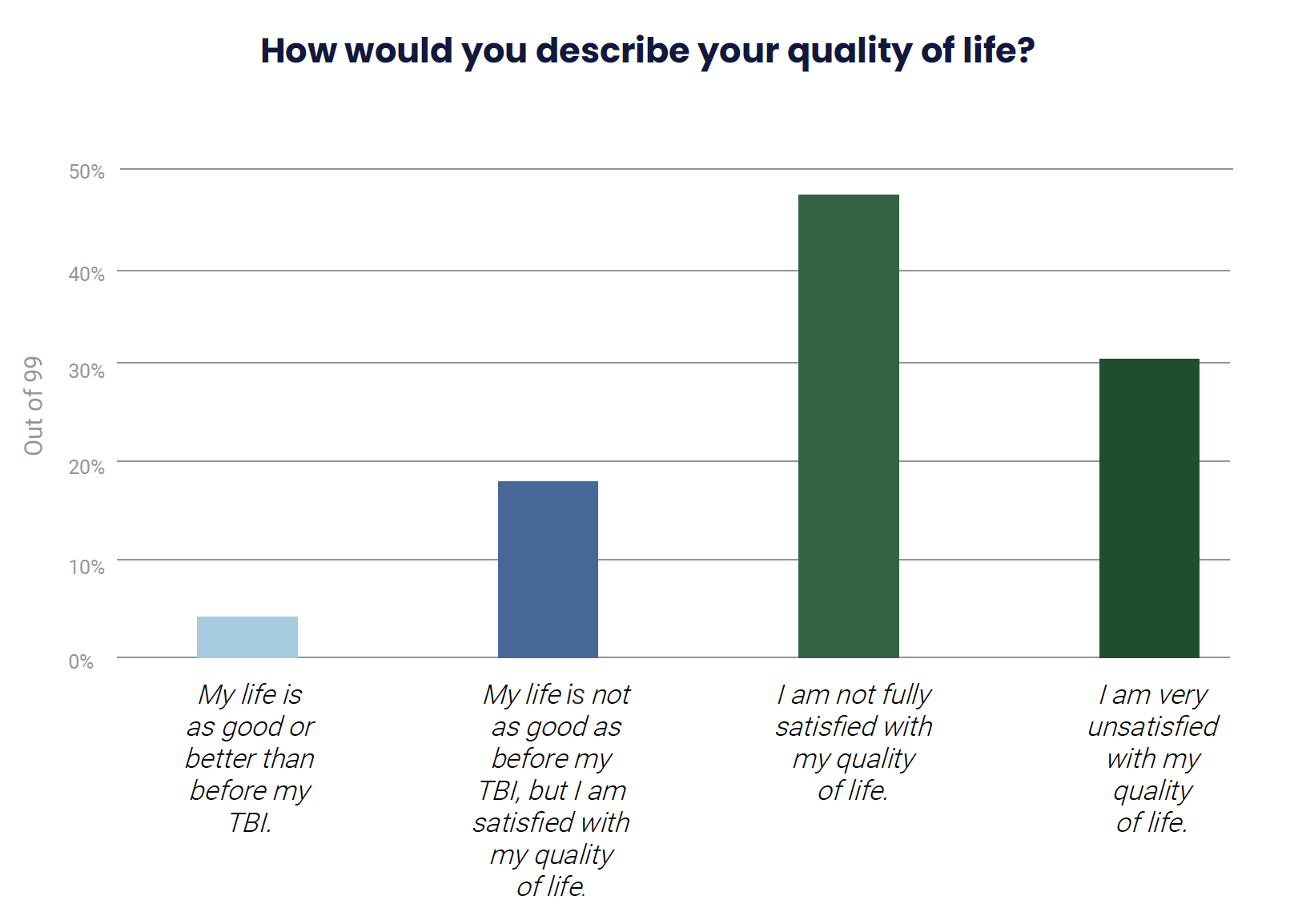
The severity of the need for community services to improve quality of life is starkly illustrated by the answer to another survey question: How would you describe your quality of life? An appalling 77% of those who responded chose “I am not fully satisfied with my quality of life” or “I am very unsatisfied with my quality of life.”
Considering that the ultimate goal of North Carolina’s transition of its Medicaid program to a managed care model [2] is to provide people with integrated care that seeks to improve the health of the whole person, it is clear that the state’s providers of Standard [3] and Tailored [4] Plans need to understand what it means to serve people with TBI and how to ensure that the whole person can achieve health and well-being.
[2] https://medicaid.ncdhhs.gov/transformation
[3] https://ncmedicaidplans.gov/
Survey Question: How would you describe your quality of life?
Answer Choices |
Percentage of Responses |
Number of Responses |
| My life is as good as or better than before my TBI | 4.04% | 4 |
| My life is not as good as before my TBI, but I am satisfied with my quality of life | 18.18% | 18 |
| I am not fully satisfied with my quality of life | 47.47% | 47 |
| I am very unsatisfied with my quality of life | 30.30% | 30 |
Disparities in TBI Treatment
While anyone is at risk for getting a TBI, some populations have a greater likelihood of dying or living with long-term problems as a result of a TBI [5]:
- American Indian/Alaska Native children and adults have higher rates of TBI-related hospitalizations and deaths than other racial or ethnic groups.
- Hispanic and non-Hispanic Black patients are less likely to receive intensive rehabilitation for a TBI when compared to non-Hispanic White patients with the same insurance coverage (e.g., Medicare). [6]
- Hispanic and non-Hispanic Black patients are less likely to receive follow-up care and rehabilitation following a TBI compared to non-Hispanic White patients.
- Individuals who are racial or ethnic minorities are more likely to have poor psychosocial, functional, and employment-related outcomes after sustaining a TBI than non-Hispanic White individuals. [7]
- People with TBIs who have lower incomes or who are uninsured are less likely to receive inpatient services, such as rehabilitation, and are less likely to receive a TBI procedure (e.g., craniectomy/craniotomy, ventriculostomy, intracranial pressure monitor placement, arterial line placement, or central line placement). [8]
[5] Gao S, Kumar RG, Wisniewski SR, Fabio A. Disparities in health care utilization of adults with traumatic brain injuries are related to insurance, race, and ethnicity: A systematic review. Journal of Head Trauma Rehabilitation. 2018;33(3):E40-e50.
[6] Meagher et al., 2015; https://pubmed.ncbi.nlm.nih.gov/25415069/
[7] https://www.cdc.gov/traumaticbraininjury/health-disparities-tbi.html
[8] Ibid.
The Prevalence of TBI
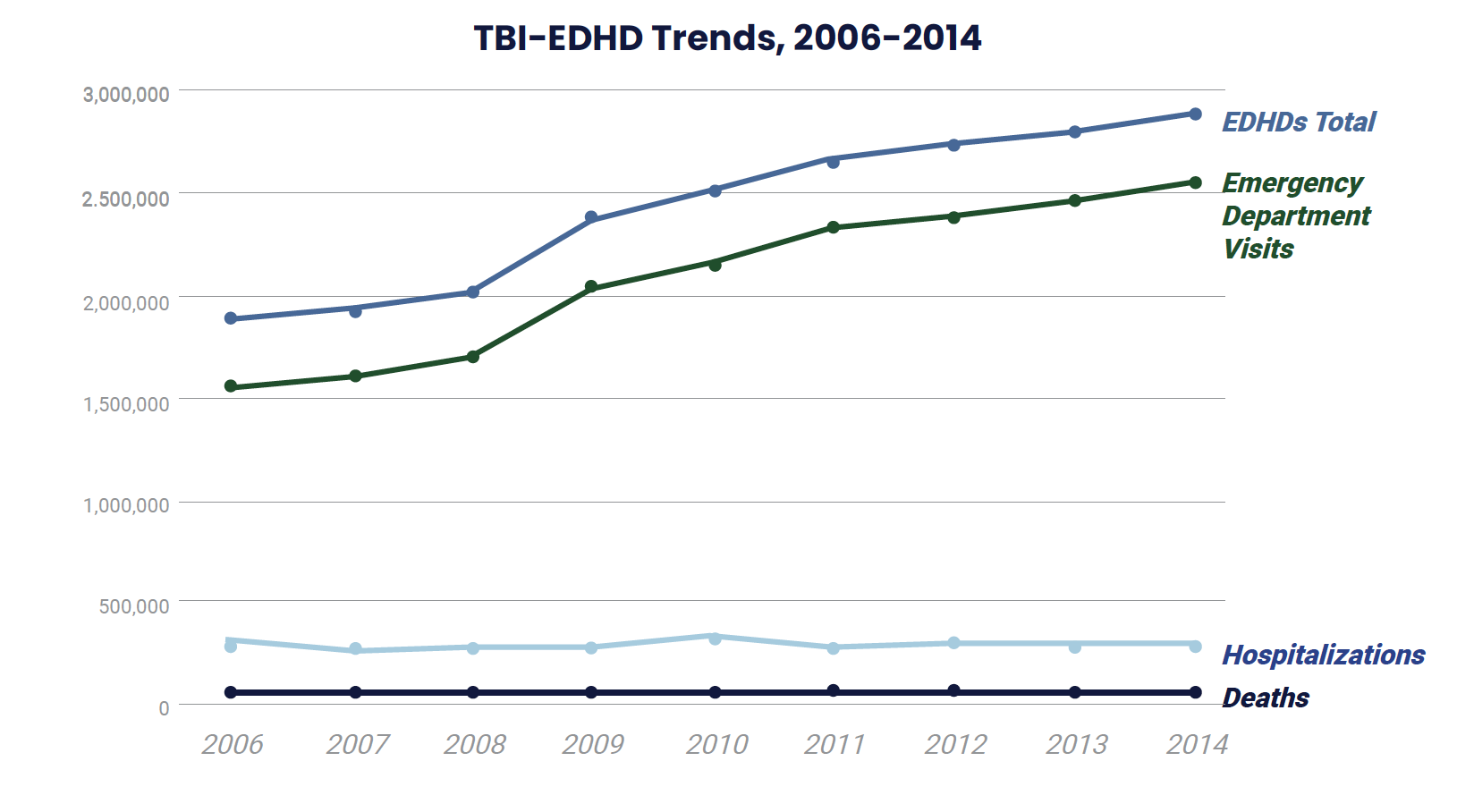
The number of total TBI-related emergency department visits, hospitalizations, and deaths (TBO-EDHDs) increased by 53% from 2006 (N approximately 1.88 million) to 2014 (N approximately 2.88 million), according to the Centers for Disease Control and Prevention.
TBI-EDHD Trends, 2006-2014
EDHDs total |
Emergency department visits |
Hospitalizations |
Deaths |
|
| 2006 | 1,884,195 | 1,551,107 | 278,655 | 54,433 |
| 2007 | 1,925,173 | 1,603,124 | 267,350 | 54,699 |
| 2008 | 2,019,166 | 1,698,326 | 267,015 | 53,825 |
| 2009 | 2,377,868 | 2,047,886 | 277,315 | 52,667 |
| 2010 | 2,521,966 | 2,143,133 | 325,996 | 52,837 |
| 2011 | 2,653,617 | 2,332,299 | 267,480 | 53,837 |
| 2012 | 2,735,909 | 2,390,167 | 290,360 | 55,382 |
| 2013 | 2,797,754 | 2,460,278 | 281,555 | 55,921 |
| 2014 | 2,877,757 | 2,532,537 | 288,420 | 56,800 |
Navigating Changing Needs
Individuals with TBI face considerable obstacles when it comes to finding the services that can improve their quality of life. At the time of their injury and during the subsequent years as the effects of the injury evolve, there is little assistance available to help them navigate North Carolina’s complex system of services.
Individuals with TBI and their families often face tremendous challenges in the immediate aftermath of an injury. Their entire world has changed, and they face a steep learning curve as they try to understand the unique physical, cognitive, and emotional effects of TBI. Survivors of a moderate or severe TBI may face a difficult road to recovery and may require services and therapies for months or years. If the individual with TBI can no longer work, the family may have lost a wage earner, and figuring out how to provide care for the individual when they come home can be difficult.
In the midst of this emotional and financial upheaval, individuals and families are also expected to learn how to navigate the system of disability services and benefits. It is a difficult process made even more complex by the fact that many agencies may require the individual, as a legally responsible adult, to initiate contact, supply information, and make decisions—even though, in the aftermath of the injury, the individual may not be physically, cognitively, or emotionally able to focus on and complete such tasks without support.
“My parents are older and have many health problems and no one will help them to help me. I would like to work at least 1 day week but have no job coach. I feel isolated a lot due to no services available.”
A 36-year-old person with a TBI in Buncombe County in response to the question, “What supports or services not covered in this survey would be useful to you?”
These circumstances speak to the need for a system to assist individuals and families in the weeks and months after a TBI to help them understand their options and make decisions. However, we heard from professionals, individuals, and family members that long-term assistance is also critical because of the sometimes dramatic changes people with TBI go through in the years following their injury.
Consider the brain’s ability to change:
— Introduction to Psychology, 1st Canadian Edition [9]
The neuroplasticity of the brain means that the physical, cognitive, and emotional functions of an individual with TBI will almost certainly change over time. As a result, an individual who, for example, is not ready for vocational rehabilitation six months after a TBI may be ready for these services a year or two later. Without assistance from a professional with deep knowledge of the system of services, the individual may not know about vocational rehabilitation or how to access the service.
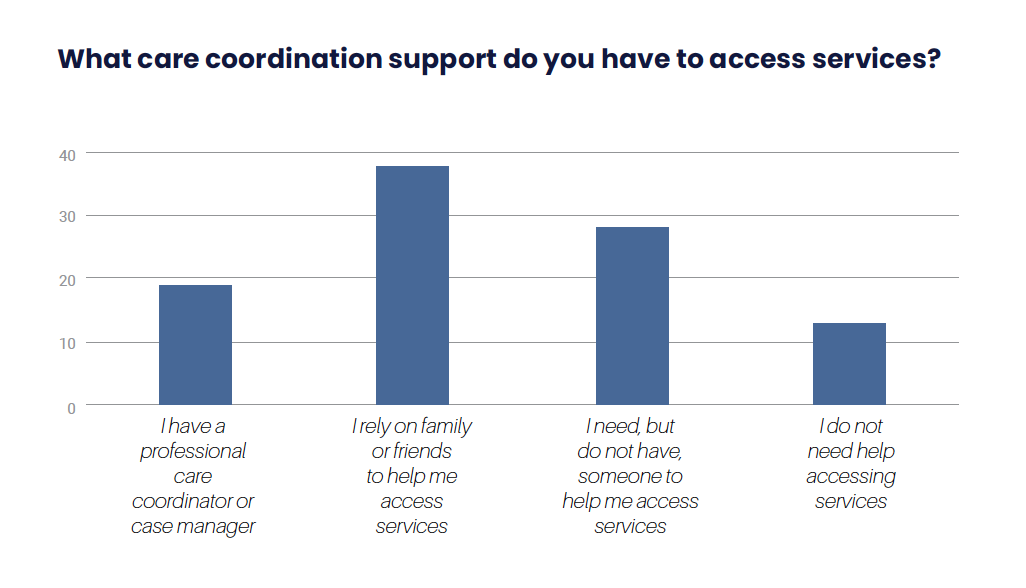
Survey Question: What care coordination support do you have to access services?
Answer Choices |
Number of Responses |
| I have a professional care coordinator or case manager. | 19 |
| I rely on family or friends to help me access services. | 38 |
| I need, but do not have, someone to help me access services. | 28 |
| I do not need help accessing services. | 13 |
Dr. Laurie Leach, the program director of the WakeMed Neuro Care Unit in Raleigh, explained that even professionals cannot predict how a patient with severe TBI will improve and grow. “There’s more and more research that suggests that sometimes for severe traumatic brain injury, the outcomes aren’t always as dreary as we anticipate they will be, and that there are some people that really can make good gains over time,” she said. “Making sure that family is understanding that too and knows how to access resources again down the road when they need to, I think, is a challenge.”
Individuals with TBI face a similar challenge when it comes to therapies. In the months after a TBI, speech, occupational, and physical therapies may help an individual regain certain skills. Those services may be available, but coverage is often limited to a certain number of visits, often an aggregate of all these treatments. [10] However, it may be years before losses in executive functioning or emotional regulation become clear. Even if the individual or their family members recognize the need for additional therapy, they may not be able to find a qualified provider, given North Carolina’s inadequate provider network. Again, they need assistance to both identify the appropriate intervention and connect with a provider.
[10] A beneficiary can receive a maximum of 27 therapy treatment visits per calendar year across all therapy disciplines combined (occupational therapy, physical therapy and speech/language therapy). NC Medicaid Clinical Coverage Policy 10A, 5.4.
Long-term Challenges of Navigating Legal and Services Systems
Sally B., 47, was in a car accident in October 2010 that caused a severe traumatic brain injury. Her parents became her guardian of the person and guardian of the estate. “After my wreck, I just remember noting it took several years for my head to start thinking again. And when it started clicking, I could begin to put things in order and figure out what I needed to do and stuff.”
Once she “started clicking” again, Sally wanted her rights restored, but she had to figure out the process herself. She wishes she had what she calls a “liaison” – someone to give her guidance and help her navigate the legal system. She told the interviewer: “Say, for instance, if you were my liaison, you’d say, “Your family are milking you dry. They’re taking all your money… If you want to get your finances back, this is what I suggest you do. If you want to get your driver’s license back so you can drive yourself to the grocery store, instead of having to pay a cab, this is what I suggest you do.”
Professionals we spoke with also noted the ongoing mental health needs of people with TBI and their families. Jennifer Myatt, a psychotherapist with Carolinas Rehabilitation, points out that the losses and dramatic changes in life following a TBI can lead to grief and depression for the individual and their relatives years later. “Everybody in the family system goes through their own grief process, and sometimes those processes can clash.”
“[S]omeone to check on me because I can’t remember anything but I look normal but I am not normal at all… I would like cognitive therapy the most because I am stupid and I am really angry all the time.
A 47-year-old person with a TBI in response to the question, “What supports or services not covered in this survey would be useful to you?”
Another even more difficult challenge can arise as an individual with TBI gets older. The Alzheimer’s Association says three decades of research has linked traumatic brain injury to a greater risk of developing Alzheimer’s disease or other forms of dementia. “[T]raumatic brain injury is a significant risk factor for cognitive decline in older adults and associated with an earlier age of onset in people with mild cognitive impairment and Alzheimer’s disease,” according to the association’s website. [11]
[11] https://www.alz.org/alzheimers-dementia/what-is-dementia/related_conditions/traumatic-brain-injury
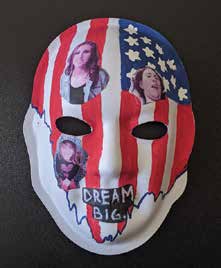
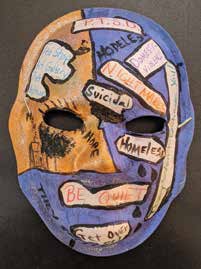
The Brain Injury Association of NC’s Unmasking Brain Injury Project promotes awareness and advocacy about brain injury. Upon request, each person living with brain injury receives and designs a mask to tell their individual journey. The masks are mounted and displayed statewide in the community. The mission of Unmasking Brain Injury is to promote awareness of the prevalence of brain injury; to give survivors a voice and the means to educate others of what it’s like to live with a brain injury; to show others that persons living with a disability due to their brain injury are like anyone else, deserving of dignity, respect, compassion and the opportunity to prove their value as citizens in their respective communities.
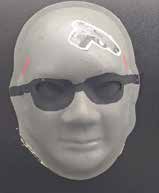 Name: Chad City: Goldsboro
Name: Chad City: Goldsboro
Brain Injury: Gunshot wound damaged my frontal lobe and destroyed both eyes.
Explanation of Mask: 2016 gun shot went through the temporal lobe, exiting the other side. The bullet destroyed my eye, leaving me blind. Also, a portion of my frontal lobe was destroyed leaving me hurt, frustrated, and angry.
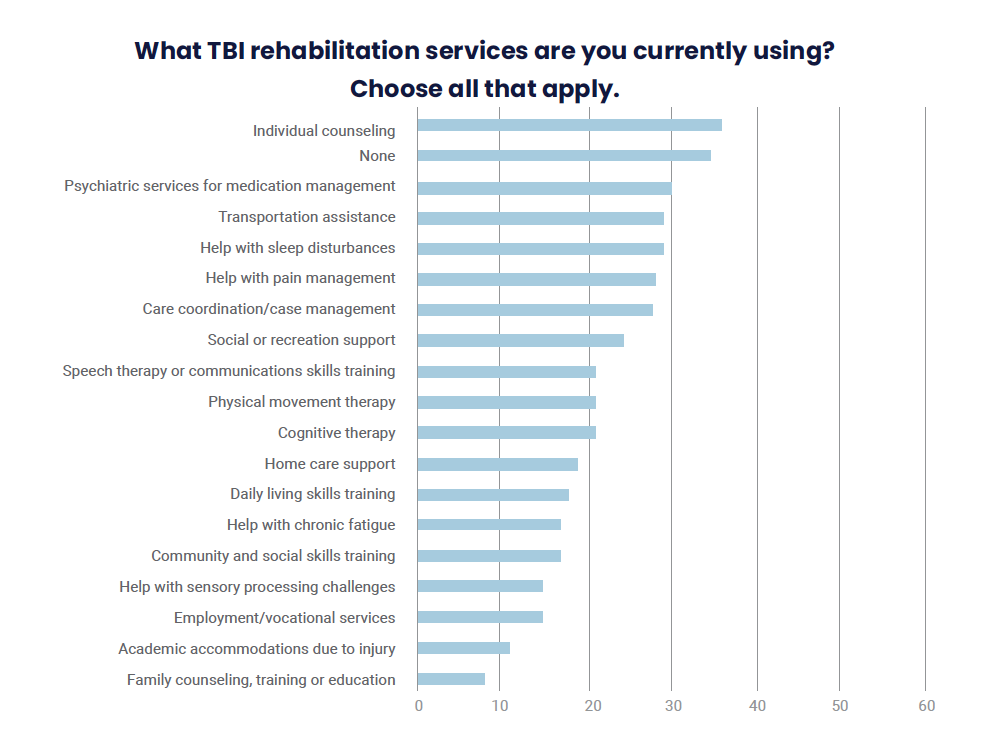
Survey Question: What TBI rehabilitation services are you currently using? Choose all that apply.
Answer Choices |
Number of Responses |
| Academic accommodations | 11 |
| Care coordination/case management | 28 |
| Cognitive therapy | 21 |
| Community and social skills training | 17 |
| Daily living skills training | 18 |
| Employment/vocational services | 15 |
| Family counseling, training, or education | 8 |
| Help with chronic fatigue | 17 |
| Help with pain management | 28 |
| Help with sensory processing challenges | 15 |
| Help with sleep disturbances | 29 |
| Home care support | 19 |
| Individual counseling | 36 |
| None | 34 |
| Physical movement therapy | 21 |
| Psychiatric services for medication management | 30 |
| Social or recreation support | 24 |
| Speech therapy or communication skills training | 21 |
| Transportation assistance | 29 |
Survey Question: Thinking about services you do NOT currently have, what TBI rehabilitation services would you use if they were available. Choose all that apply.
Answer Choices |
Number of Responses |
| Family counseling, training, or education | 32 |
| Academic accommodations due to injury | 22 |
| Employment/vocational services (help getting or keeping a job) | 38 |
| Help with sensory processing challenges | 35 |
| Community and social skills training | 35 |
| Help with chronic fatigue | 30 |
| Daily living skills training | 28 |
| Home care support | 17 |
| Cognitive therapy (for attention, memory, initiation, problem solving, planning, etc.) | 55 |
| Physical movement therapy | 35 |
| Speech therapy or communication skills training | 21 |
| Social or recreation support (help with loneliness, opportunities to be around other people) | 53 |
| Care coordination/case management (a professional to help arrange the services you need) | 42 |
| Help with pain management | 15 |
| Help with sleep disturbances | 31 |
| Transportation assistance | 18 |
| Psychiatric services for medication management | 14 |
| None | 12 |
| Individual counseling (depression, anxiety, anger, or substance abuse, etc.) | 50 |
North Carolina’s TBI Waiver
For years, North Carolina’s state funding for TBI services has remained stuck at about $2.1 million— only enough to provide services to about 150 people. [12] With such a tiny pool of potential patients, providers have had no incentive to pursue training and certifications in TBI, resulting in a severe lack of TBI-specific services.
North Carolina’s creation of its three-year TBI waiver initiative program was a critical step toward improving care of people with TBI. Through this program, the state can provide a wide range of Medicaid-funded services to people with TBI. The initiative program launched in September 2018 in only one of the state’s seven local management entities/managed care organizations (LME/ MCOs). Alliance Health was chosen as the initiative LME/MCO, so only people in its catchment area— Wake, Durham, Cumberland, and Johnston counties—have been eligible for the waiver.
[12] North Carolina’s last state budget, passed in 2017, allocated $2,373,086 in recurring funds to support TBI services. The budget allocated $359,218 for “contracts with the Brain Injury Association of North Carolina, Carolinas Rehabilitation, or appropriate service providers to assist families in accessing the continuum of care and to provide educations programs on brain injury prevention, intervention, and care.” The remaining $2,013,868 went to support residential programs for people with TBI and support requests from individuals with TBI, which go through the LME/ MCOs. https://files.nc.gov/ncdhhs/TBIStateFunds2017.pdf
Services Available under North Carolina’s TBI Waiver as listed on Alliance Health’s flyer for the TBI waiver
- Home and Community Services
- Cognitive rehabilitation
- Life-skills training
- Personal care
- Resource facilitation
- Respite
- Day Services
- Supported employment
- Community networking
- Day supports
- Adult day health
- Behavioral or Specialty Services
- Allied health (physical therapy, occupational therapy, speech therapy)
- Specialized consultation
- In-home intensive supports
- Residential
- Residential supports (group home or Alternative Family Living setting)
- One-time or As-needed Services
- Assistive technology
- Home modifications
- Natural supports education
- Vehicle modifications
- Community transition
- Crisis services
The initiative program ended in April 2021, and sadly, it helped very few people. The program was supposed to serve 107 people by the end of its third year. As of January 5, 2021, Alliance was providing waiver services to only 41 people. North Carolina is expected to submit an application to the federal Centers for Medicare and Medicaid Services (CMS) to renew the program, but it will continue to be limited in its geographic scope.
There are several reasons why the waiver has not been more widely used within the Alliance catchment area. Simply finding and connecting with people who could benefit from the waiver is a challenge because the state has not kept track of people with TBI. Furthermore, the application process for the waiver is arduous and takes months to complete. Many people with TBI have diminished memory and cognitive functions that make searching through medical records, reaching out to former providers and hospitals, and compiling their financial history incredibly difficult.
Alliance has recognized this problem and has taken some action. According to the quarterly report that the DHHS submitted to the state legislature in January 2021 [13], Alliance employs a TBI Guide to help people who are interested in the waiver to gather the clinical documentation needed to determine eligibility, and it has “established a TBI Guide relationship with a nonprofit organization to assist TBI individuals.”
An Inadequate Provider Network
The quarterly legislative report on the waiver also said, “There are currently 24 providers in Alliance’s TBI provider network and there is at least one provider per TBI waiver service within the Alliance Network.” That is 24 providers for a catchment area that has approximately 2 million people and spans 120 miles from the northwest tip of Durham County to southeast Cumberland County. It could take someone in Durham more than two hours to get to a provider in Cumberland County. This lack of providers is a significant obstacle to care.
In other words, even with the benefit of these waiver services, the system fails people with TBI.
Janine Pearson, MS, CCC-SLP, is the owner and lead speech pathologist of Cognitive Rehabilitation Services in Wake Forest, NC. She says that in order to be most effective, therapists need to be specifically trained to work with people with TBI. A therapist without such training may not be aware of certain challenges, such as cognitive fatigue.
“Cognitive fatigue is something that, if you have not had a lot of experience with brain injury, is really hard to understand. Someone with a brain injury can be very alert, pleasant and able to complete a task when their brain is not tired. Then an hour later if they tried to replicate that task, it could be impossible. They could have anger outbursts. All of these negative things can happen just because their brain is tired.”
North Carolina’s State Action Plan for People with TBI acknowledges the need to grow this astonishingly meager provider network. The following is one of the objectives in the plan under the goal “Resource Access and Engagement”:
Objective 1. Explore opportunities for advocacy to allow for recommendations related to public policy and legislation.
Measure 1: Investigate gaps & needs within the NC service system for individuals living with TBI, including potential barriers to accessing services, long-term supports, residential options, employment, transportation, care coordination or disparities for historically marginalized populations.
Measure 2: Identify and advocate for recurring funding opportunities for individuals living with brain injury to help the TBI service infrastructure and sustain the continuum of TBI care.
Unfortunately, this “action” plan does not provide any guidance on how to engage providers, educate them about TBI, and encourage them to get the training necessary to become a quality provider of TBI services.
There is training available, but the current system requires providers to absorb the costs of the training. For example, according to the quarterly waiver report, “Alliance contracts with the Brain Injury Association of North Carolina (BIANC) to offer providers and their staff access to the Certified Brain Injury Specialist (CBIS) Certification training program,” but in order to gain CBIS certification, a professional must pass a standardized exam and have completed 500 hours of paid work experience with brain injury in the preceding three years.
“Well, the services mentioned in the survey were great, however, there are not enough trained professionals that know how to help TBI here in Wilmington, North Carolina. [T]his runs from Mental Health, Colleges, Vocational Rehabilitation Services, police officers, court systems……all aspects of daily life.”
A 42 -year-old person with TBI in response to the question, Please list any gaps in services you have encountered that were not covered in the survey questions.
Regardless of whether a provider wants to obtain the certification or just wants to educate themselves and their staff about TBI, as noted there is one significant obstacle—money. Providers cannot bill Medicaid, Alliance, or the state for time spent on TBI training. Certainly, many providers who work with people with intellectual and developmental disabilities, people with dementia, or people who have had strokes could be able to use their skills to help people with TBI if they had some additional training on the specific needs and challenges facing that population. But the lack of funding for services and financial incentives for providers is a significant barrier to providers who otherwise would pursue such training.
Coping with Depression and Anxiety
Elijah D. was born, raised, and still lives in Thomasville, NC. He was riding a scooter when a truck hit him in 2011. Today, he is in his early 50s, and his mother helps to take care of him.
Elijah has significant challenges with both depression and anxiety. He has memory problems, and his fear that he will forget something important can trigger panic attacks. For example, Elijah has forgotten to turn off the kitchen stove in the past. “Then that gave me a panic attack, because I was scared that I could’ve burnt my house down,” Elijah said. “I could’ve burnt my dog. Or I could’ve burnt somebody, or Mama could’ve went in there and it caught on fire… I’ve had a panic attack thinking about it… I mean, I know I made, I already made my tea and everything. But I still… I’ll get up out of the living room and go in the kitchen to make sure there’s nothing sitting on the stove.”
“I get depressed a lot, too,” Elijah continued. “I feel like, I feel like me forgetting things. You know, me wanting to do things but can’t do things because I ain’t got the way to do things. I sit there and I sit there. I think about it, think about it, think about it and I start, I start crying. Tears running down my face. Because I can’t do it on my own.”
Elijah sees a neurologist quarterly who, according to Elijah and his mom, has been helpful for advice and medication management. However, Elijah has never received consistent, direct counseling from a mental health professional to address his anxiety, panic attacks, obsessive-compulsive tendencies, and depression.
 Name: TJ City: Jacksonville
Name: TJ City: Jacksonville
Brain Injury: TBI sustained as passenger in private motor vehicle while U. S. Marine on active duty, Okinawa 1976.
Explanation of Mask: Camo pattern cut from my uniform, one of many from 28+ years active duty. Blue side = cold, tolerances changed, suppression. Spike at location of impact, where pain begins and penetrates into brain. Stiches between camo into Blue represent efforts to tie my life together, before and after injury. Dark spot above eye is where pressure lingers after lightning flashes (orange painted lines with flecks of glitter for heat). Closed lips because sometimes I cannot express myself clearly; sometimes I think things but I do not want to say them. BIANC has been a very big help in assisting me learn more about TBI, my condition, and providing an opportunity to help others.
From the Brain Injury Association of NC’s Unmasking Brain Injury Project.”
Creating a Better Future for People with TBI in North Carolina
North Carolina must do much better for its residents who have a TBI. They are our neighbors, colleagues, friends and families, and should be able to pursue a life of opportunity and growth. The state must help to improve the quality of life for people with TBI, but doing so will take a statewide, rather than regional, approach.
Recommendation #1 – Invest in Identifying People with TBI and Their Needs
North Carolina’s 2021 State Action Plan for People with TBI admits, “North Carolina’s population-wide data on TBIs is limited.” Unfortunately, “limited” is an understatement. Because the state delegated identifying and tracking those people with TBI to its seven LME-MCOs, there is no centralized, standardized data to help state leaders understand the scope and needs of this population. And because identifying more individuals with TBI would reveal the extent to which this population is underserved, LME/MCOs currently lack the impetus to engage in vigorous identification efforts.
Even in those settings where North Carolina should be able to easily identify and track the prevalence of TBI, such as state operated healthcare facilities, prisons, and jails, it has not kept track of the number of people who might benefit from TBI specific services. We support efforts to identify people with TBI in inpatient settings and in jails and prisons.
Using the CDC’s estimate that two percent of people in the United States have a TBI, the North Carolina State Action Plan assumes that approximately 208,000 people in the state have a TBI. However, the only state-specific demographic data that the action plan cites are for the 41,398 individuals with TBI who received behavioral health services in state fiscal year 2019. The fact that this total includes more women (22,066) than men (19,332), even though men have a higher rate of TBI, illustrates the state’s failure to collect comprehensive data on the incidence of and individuals affected by TBI.
The result of the failure to identify and track people with TBI is that today, tens of thousands of North Carolinians who need support and services because of a TBI are left to struggle on their own or must rely on family members who simply may not be equipped to deal with the strain and challenges of caregiving over the long term.
Recommendation #2 – Invest in the Creation of a High-Quality Network of Providers
There is some good news – North Carolina has already identified and understands the services that people with TBI need to lead healthy, productive lives in their communities. As noted earlier in this report, when the state created its TBI Medicaid waiver, it listed those critical services.
The bad news is that the network of providers that offer any of these services to people with TBI is woefully inadequate in every part of the state.
Providers require training in order to serve people with TBI. What they know from serving others with cognitive challenges may be a good foundation, but it is not enough to enable them to provide high-quality services to people with TBI. A person who suffers a TBI as a young adult has different challenges and needs than a person who is born with Down syndrome or an elderly person who has had a stroke.
BIANC has created training modules to help prepare professionals to work with people with TBI. But the state has failed to pair those trainings with funding that pays providers of a wide range of services – from psychiatric treatment to direct care – to take those trainings. Simply put, business owners are not going to pay their professionals and staff to take training unless there is a way for them to bill the state for that time.
“I needed a patient advocate desperately in the early months of being at home after discharge. I did not have anyone. My brains were scrambled and I did not even know what services were available to me in order to ask for them. A patient advocate could have helped me with this and perhaps I would not have lost so much of what I had worked my entire adult life for.
A 47-year-old person with a TBI in Wayne County in response to the question, Please list any gaps in services you have encountered that were not covered in the survey questions.
Recommendation #3 – Implement Long-term Case Management for People with TBIs
The capabilities, needs, and challenges of people with TBI change over time. Throughout this report, individuals with TBI and the professionals who work with them expressed frustration over not knowing what services are available and struggling to navigate the system of care. It is unfair and unkind to expect individuals and families dealing with the immediate aftermath of a TBI to absorb information not only about the immediate mental and physical impacts, but also about all of the services and systems they may someday need to access.
Having long-term case management provides important benefits to individuals with TBIs, their families, and the state of North Carolina. A case manager with expertise in TBI can help individuals identify changes in their cognitive, mental, and physical health and help them access services that may enable them to move toward greater independence, community integration, and life satisfaction.
Struggling to Provide Services
Marty Foil’s brother Phillip suffered a severe traumatic brain injury in 1984. After a decade of searching for a therapeutic, community-based place for their son to live and thrive, Phillip’s parents decided to start their own program. They recruited Marty to lead the project, and in 2006, their first day program opened.
Today, the Foils’ non-profit organization, Hinds Feet Farm, has day programs in Huntersville and Asheville and two residential facilities. Marty serves as the executive director. “We’re member-focused, member-driven, and holistic in our approach,” Marty Foil explained. “That means that our responsibility as staff is to respond to our members’ physical, mental, emotional, and spiritual needs.”
Marty says funding for Hinds Feet Farms is complicated and involves multiple systems. “I’ve got state TBI dollars, I’ve got Mecklenburg County contracts, I’ve got some Medicaid innovations, I’ve got private pay, I’ve got neuro community care, pass through dollars, Wounded Warriors, I’ve got six funding streams to make things work.”
Marty points out that because of limited state funding and low reimbursement rates, his organization earns considerably less money than developmental disability organizations for providing the same or similar services. “I’m looking for parity across the disability groups and there’s no parity.”
Marty continued, “Serving the people that we’re serving is not a burden. What is a burden is knowing that there are so many more that you want to serve and realizing that you don’t have the fortitude left to do it. That hurts. I love to do it. I love to do it.”
 Name: Kimmy City: Apex
Name: Kimmy City: Apex
Brain Injury: Car accident
Explanation of Mask: I am unable to speak now. I will never give up. I’m tired and I’m confused. Where is my little girl, Rory? Why are all my friends married, with children now? I want my life back the way it was. What day is it? Where are you Rory? Why does her dad have her and not me? Where did he move with his new wife? I hear everyone. Mom asked me a yes/no question. How do I get the yes out? Damn, I’ve got this. I am going to walk one day. Yes, of course I am. I’m an overcomer. I’m an Army Captain. I’m a paratrooper. I’ve served in combat! Where are my friends? I’m tired. I want to see my Rory.
 Name: Loretta W. City: Raleigh
Name: Loretta W. City: Raleigh
Brain Injury: I was living in an Abusive Household while in the Military and felt I could not get out. My husband was also a soldier. I felt I was in danger every day
Explanation of Mask: My mask is divided into sections about: How the Brain Injury affected me, How I am presently coping with it, and How I want my outcome to be. I felt very alone, embarrassed, invisible and I spent time in a Mental Health Hospital in Orlando, Florida. I was told that “They Won’t Believe You!” Those words cut worse than anything ever because after 11 years of my fight with disability, it proves that those words were right.
From the Brain Injury Association of NC’s Unmasking Brain Injury Project